With the completion of a massive, $10 million renovation project, the Dwyer Healthcare Simulation Center will be operational for the fall 2024 semester. Nursing and radiography students will enjoy vastly upgraded facilities in Parkside Hall.
Dwyer Healthcare Simulation Center to debut in Fall 2024
The new simulation center is a win-win for our students and the community. Roughly 90 percent of our graduates from the radiography program stay in the area,” said program director Maryann Oake, clinical associate professor of radiologic sciences. “These upgrades raised our standard to a whole new level, greatly increasing the quality of educational experiences and hands-on application. It all helps equip our students to be stronger healthcare leaders in our community.
Radiography students complete clinical practicums at area healthcare facilities and outpatient facilities.
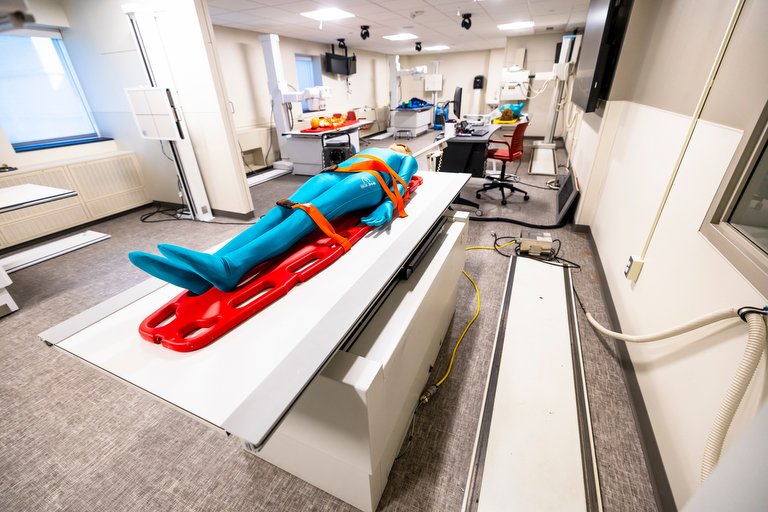
New equipment for the radiography program includes two state-of-the-art energized x-ray labs, C-arm surgical equipment, a fully functional portable x-ray unit, practice manikins, and various quality-control equipment.
"With the new equipment, students can make mistakes, identify the problem, and correct the issue all in the educational environment,” said Rory Langton, clinical assistant professor and clinical coordinator of radiologic and imaging sciences. “This will dramatically help students increase confidence and knowledge prior to entering into the clinical setting."
Video cameras will record every session in the new center, so students will be able to review everything that happened in a simulation, a debriefing, and even any conversation that has been held in the rooms. This should prove an invaluable resource to any student who would like to go over a detail an extra time.
Clinical Associate Professor Amy Gretencord is a 2003 graduate of the IU South Bend radiography program, so she has the institutional memory to appreciate the difference between then and now.
“When I was a student here, we did not have energized equipment for practicing skills before going to clinical and practicing on real patients,” Gretencord said. “Now, students will have the opportunity to take x-rays on manikins in a controlled environment. This is going to provide so many possibilities for the students in the courses I teach. I’m excited for the future of the program and what this will do for the community.”
The sonography lab has received new equipment, and students will be able to safely practice those procedures with ultrasounds by using each other as practice patients. X-rays, however, require manikins. There is no safe dose of radiation, so being able to simulate positioning and patient-care procedures in a safe environment is imperative.
Life-sized manikins have been acquired for use in the medical imaging labs, including adult-sized, pedriatric-sized, and an infant. Two models are state-of-the-art “anthropomorphic phantoms.” Between the two of them, the phantoms can simulate 60 traumas and pathologies. Students can run tests on the phantoms, using modalities such as CT scans, x-rays, and fluoroscopy, as the manikins present symptoms that can range from bullet wounds to broken ankles to pelvic fractures. The phantoms’ realistic anatomy, lungs, and skeleton are detailed down to the ball and socket joints of their shoulders. This means that they “behave” just as a person would while being positioned on the examination table.



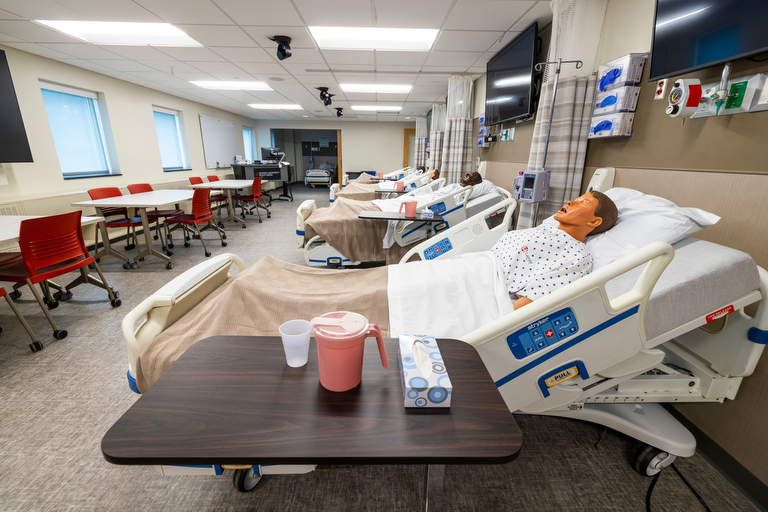
On the second floor, nurses can attend to another kind of manikin. One of its default settings is Juan, a three-year-old boy presenting symptoms of a ruptured appendix. He’s in pain, he’s dehydrated, and he does not speak English. His voice comes from an instructor, using a microphone in the adjacent observation room. The nurses need to diagnose and treat his physical ailments, while also negotiating a checklist of personal variables. Someone needs to speak Spanish with Juan and a family member. They need to balance pain management (meds) with emotional responses (offer Juan a teddy bear). They need to determine if there are allergies, answer questions about insurance, and handle any number of other situations they will face in a clinical setting.
At the end of 2023, there were approximately 6,000 unfilled RN positions in Indiana. None of the Dwyer school nursing graduates will be forced to look for out-of-state work. Not surprisingly, 90% of IU South Bend graduates stick around to work professionally in the greater South Bend-Elkhart region.
In many cases, students will train in the same hospitals and clinics where they will later work as professionals. Barbara White, assistant dean in Nursing with the Vera Z. Dwyer School of Health Sciences envisions deepening bonds with Memorial Hospital, Elkhart General Hospital, Saint Joseph Health System, and Goshen Health.
“We want to open the doors to all four of those places, so that they can feel free to come and use our space for their own staff training,” White said. “This should also lead to interprofessional education collaborations, where our students are interacting with professionals.”
“The clinical sites rely on our grads to staff their hospitals,” said assistant clinical professor Taryn Liechty. “So the relationship is already there and it’s already strong.”
“The students complete many hours in the hospital before they graduate, so they become very familiar with the local hospitals,” White said. “Because we’re in the midst of a nursing shortage, nurses in their last semester can get hired right in the hallway.”
The opportunities are so plentiful that White and her colleagues make a point of recommending that young nurses not just take the first offer that comes their way. A bad first experience can lead to burnout, with 40% leaving the field after the first year, even in a post-Covid environment. The virus wreaked havoc on morale.
“It’s going to take a long time. It’s going to take years,” Liechty said. “It’s going to take another generation of nurses to come in and help bolster up the work force and bolster up the profession.”
“Our profession needs their young energy, their idealism,” White said. “In a video we show to the students, a nurse from an ER setting says that they don’t have any lily flowers working there. We’re creating strong, independent, hard-working, intelligent, assertive, compassionate, resilient nurses. No lily flowers.”
Back in the simulation center, observers can monitor the simulation areas unseen, behind a one-way window. Debriefing rooms are juxtaposed with the simulation rooms and observation rooms, so everyone can convene and review the results of the simulation immediately upon its completion.
“There is nothing a student can do in the simulation room that will make them fail. It’s a safe place to learn because the students know that they are allowed to make mistakes in that room,” Liechty said. “In the debriefing, which usually lasts two or three times longer than the sim itself, we break down all the information and we think about how we can do something better the next time. Using manikins instead of real people, we can make their situations and symptoms a little bit more severe, which tests the nurses a little bit more, gets them away from their safety net.”
“What they cannot do in the real world is make a mistake,” White said. “Taryn’s never going to let them make a mistake in the PCU (Progressive Care Unit) at Memorial. In simulation, they can make a mistake and then think through their decisions, without anybody in their ear.”
Afterwards, in a student-led, instructor-facilitated debriefing, there will be time to break down the simulation, identify how the mistake was made, and recommend better approaches. White stresses that there are two crucial concepts in this kind of nurse training: thinking in action and thinking on action.



Thinking in action is thinking in the moment, and in the simulations we’re trying to get them to think in action better,” White said. “Thinking on action is the reflection we’re doing in the debriefing, and we encourage them to think on action for the rest of their careers.”
This can mean asking questions about what they might have missed in a diagnosis, what kinds of meds are being chosen, the timing of the meds, or any number of other scenarios that could benefit from a never-ending process of refinement.
Why are some people nurses for 30 years and they are only competent, whereas other nurses are excellent within five or ten years? Some of it is experience, but a lot of it is thinking on action,” White said.
Some students will prefer to remain in an intense, white-knuckle simulation, and will learn best in high-pressure scenarios. Other students might benefit from slowing things down in the moment, and they are permitted to call a “time out.” In that case, the simulation is paused and the observation team comes in to consult right then and there.
It’s possible to become overwhelmed,” White said. “Psychological safety in simulation is something that’s important because anxious and stressed students don’t learn as well.”
Alexis Wilfing, a second-year nursing student from Plymouth, Indiana, is eager to explore the possibilities that the new space has to offer. She originally matriculated at Saint Mary’s College, focusing on chemistry and a Pre-Med track, and transferred to IU South Bend after a change of mindset.
I decided that I wanted to spend more time with patients than a doctor does,” Wilfing said. “I realized that I really needed to be a nurse.”
Wilfing has begun her nursing education in the previous facilities, and she has already appreciated the value of the simulation process.
They make it clear that this is the time to make the mistakes. This is the time to mess up, because we can talk about it,” Wilfing said. “They’ll show us what we could have done differently, and then the next time, there’s the fantastic feeling of, ‘Oh, I know just how to fix that.’
The expanded layout of the physical space in the units is a simulation in its own right, resembling real-life clinics and hospitals far more accurately than before. A typical process they replicate is when a nurse is filling a prescription, then triple-verifying the med and the dose, then administering to the patient. In a real-life hospital, this happens in multiple stages, each with an unpredictable set of distractions and complications, but the old Sim lab had everything happening in the same area.
“The whole supply room was right next to the bed,” Wilfing said. “You’d pretend to go off to the side in a hallway, checking it again. Now that it’s actually down the hall, it’s much more like the hospital.”
A radiography or nursing degree in the present job market allows a person to have the privileges of being able to work practically anywhere. That kind of social mobility is empowering, and it can also mean that nurses and radiographers can use that power to choose to stay near their family and the area where they grew up. Vera Dwyer expressed specifically that she hoped her gift would benefit the immediate region, so every Titan graduate who sticks around is helping to honor that wish.
“There’s something special about this nursing program, and I love where I am right now,” Wilfing said. “I like living here, and I plan to stay.”

The Vera Z. Dwyer Charitable Trust, local READI funds, and the Community Foundation of St. Joseph County raised the majority of the $10 million needed for the renovation. Further funding is still required, including room-naming opportunities.
Learn more about the Sim Center campaign and giving opportunities.
For more information on the Sim Center campaign contact Dana Rassas Jojo at 574-520-4454

